California Midwives Are Essential Maternity Care Providers
Midwives Play A Crucial Role in Ensuring Safe Maternity Care in California
Robust studies in recent years show that excellent birth and infant outcomes result when midwives are a part of an integrated system of care committed to delivering whole-person safety. (1,2,3,4,5)
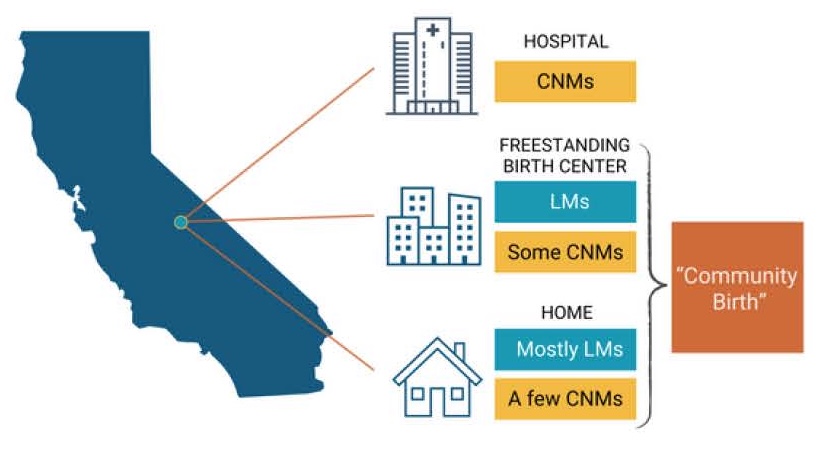
Types of Midwives in California
- Certified Nurse-Midwives (CNMs)
- Licensed Midwives (LMs)
- Total number of midwives in CA (CNMs and LMs combined) = 1,600
Education and Regulation

Scope of Practice
- Low-risk pregnancy, labor, and birth in hospitals, freestanding birth centers, and homes
- CNMs and LMs care for patients who meet the criteria of “low-risk” as defined by the Board of Registered Nursing and the Medical Board of California, respectively; CNMs and LMs are obligated to transfer-higher risk patients
- Management of “normal” changes of pregnancy, including miscarriage care; medication or aspiration abortion in the 1st trimester (CNMs only)
- Well-newborn care
- Well-person gynecologic care, including sexually transmitted infection (STI) care, contraception, and care during menopause
- CNMs and LMs are independent providers who consult, collaborate, and transfer care when necessary as indicated by the patient’s risk level and medical conditions
Environments of Care in California
What the Midwifery Model of Care Looks Like in Community Settings in California*
- Comprehensive care management and attention to health-related social needs with necessary referrals (e.g., food assistance, housing, intimate partner violence, etc.)
- Trauma-informed care is standard
- Continuous risk assessment with early referral to physician care if medical needs arise; ability to consult with a physician is essential
- Collaboration with doulas and other professionals who can improve wellbeing and enhance care
- Personalized education for nutrition, exercise, lactation, urgent maternal warning signs, and childbirth
- Hour-long prenatal visits
- 24/7 access to a midwife whom the patient is well acquainted with Continuous presence during labor and birth
- 3-5 hour-long postpartum visits in the first 6 weeks (the time when most maternal mortality occurs)
- Dyadic care (patient and baby cared for together in postpartum period)
- One-on-one lactation support as needed and for as many visits as needed
*Community midwifery = midwifery care in homes and freestanding birth centers
Philosophy of Midwifery Care
As defined by the International Confederation of Midwives(6)
The International Confederation of Midwives' philosophy of midwifery care affirms pregnancy and childbearing as typically normal, physiological experiences that are deeply meaningful to women and their communities. Midwives are ideal providers for low-risk people, offering holistic, continuous, and collaborative care that supports women's health, rights, and self-determination. This respectful, personalized care builds confidence in childbirth, grounded in ethical principles, individuals’ backgrounds, and an understanding of women's comprehensive experiences. Competent midwifery is continuously informed by education, scientific research, and evidence.
Collaboration Is Essential
Studies show that outcomes are better for low-risk, essentially healthy people receiving community-based midwifery care when midwives are part of an integrated healthcare system where they can practice to the top of their training, easily consult with physicians when medical issues arise, and efficiently transfer to physician care and/or higher levels of care as needed, as compared to patient and population outcomes when midwives are not fully integrated into the healthcare system. The Community Birth Partnership Initiative encourages collaboration across care settings and between different provider types (e.g., between physicians and midwives), promoting team-based care to improve outcomes for low-risk individuals giving birth in community settings.
References
- Nethery E, et al. Birth Outcomes for Planned Home and Licensed Freestanding Birth Center Births in Washington State. Obstetrics & Gynecology. 2021. https://doi.org/10.1097/AOG.000000000000457
- CMS Strong Start for Mothers and Newborns Initiative. 2018. https://www.cms.gov/priorities/innovation/innovation-models/strong-start
- Vedam S, et al. Mapping Integration of Midwives across the United States. Plos One. 2018. https://doi.org/10.1371/journal.pone.0192523
- Cheyney M, et al. Outcomes of Care for 16,924 Planned Home Births in the United States: The Midwives Alliance of North America Statistics Project, 2004 to 2009. J Midwifery Womens Health. 2014;59(1):17-27. https://doi.org/10.1111/jmwh.12172
- Bovbjerg ML, et al. Planned Home Births in the United States Have Outcomes Comparable to Planned Birth Center Births for Low-Risk Birthing Individ- uals. Med Care. 2024;62(12):820-829. https://doi.org/10.1097/MLR.0000000000002074
- International Confederation of Midwives. Core Document: "Philosophy and Model of Midwifery Care". https://internationalmidwives.org/wp-content/uploads/eng-philosophy-and-model-of-midwifery-care.pdf.